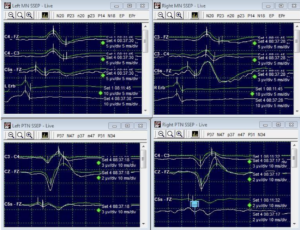
We have a patient, a 39-year-old woman, who came to the emergency room complaining of a very intense headache and vomiting. After conducting a CT scan, we found that she had bleeding in the area surrounding the middle cerebral artery on the right side of her brain. Additionally, there was an aneurysm in a blood vessel called the posterior communicating artery. To address these issues, we brought the patient into the operating room for a surgical procedure called a craniotomy. During this operation, we aimed to repair the aneurysm by placing a clip on it. Before making any incisions, our monitoring technician successfully recorded sensory evoked potentials (SSEP) in all of the patient’s limbs. This data helps us assess the integrity of the patient’s spinal cord and nerves. Throughout the surgical procedure, starting from removing a piece of the skull (called a bone flap) to dissecting around the aneurysm, the SEP data remained stable and consistent. This indicates that the patient’s nervous system was functioning properly and undisturbed by the surgical steps taken so far.
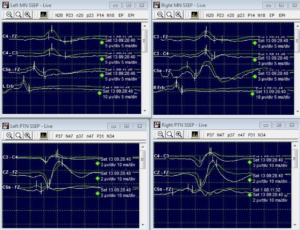
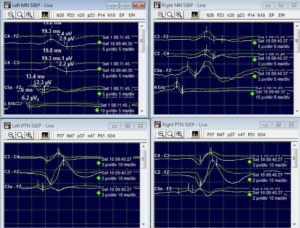
During the initial process of clipping the aneurysm, we observed a drop in the cortical responses of the left median nerve SSEP (sensory evoked potentials). However, the subcortical and peripheral responses remained Unaffected. To put it simply, when we were working on the aneurysm, we noticed a change in the way the patient’s brain was responding to sensory stimulation on the left side. Specifically, the signals from the area of the brain responsible for processing touch sensations in the hand showed a decrease. However, the responses from deeper parts of the nervous system and the nerves in the hand were still functioning normally.
This change in cortical responses could be an indication that the surgery is impacting the function of the patient’s sensory pathway in the brain. It’s important for us to closely monitor this situation and take appropriate measures to ensure the patient’s well-being throughout the procedure.
The surgeon was alerted to the change in the left median nerve SSEP (sensory evoked potential) and took immediate action. They adjusted the position of the clip that was placed on the aneurysm. As a result of this repositioning, we observed a return to the baseline or normal response of the left median nerve SSEP. In other words, the signals from the area of the brain responsible for processing touch sensations in the hand returned to their normal patterns.
By repositioning the clip, the surgeon was able to restore the proper blood flow and reduce any potential compression or disruption to the nerves. This adjustment ensured that the patient’s sensory pathway in the brain was functioning as expected once again.
This intervention highlights the surgeon’s attentiveness and skill in responding to changes observed during the surgery. It’s important to address any deviations from the normal responses promptly to protect the patient’s neurological function and overall well-being.
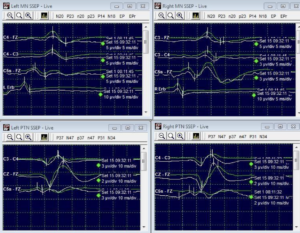
During the procedure, additional clips were placed on the aneurysm. However, this unfortunately led to a complete loss of cortical responses in the left median nerve. The neuromonitoring team, responsible for closely monitoring the patient’s nervous system during surgery, immediately detected this significant change and promptly alerted the surgeon.
To simplify, when the surgeon placed more clips on the aneurysm, it caused the brain’s ability to process touch sensations from the left hand to completely disappear. This is a crucial finding that needed immediate attention. The vigilant neuromonitoring team played a crucial role in recognizing this adverse event. Their expertise in monitoring and analyzing the patient’s sensory responses allowed them to swiftly identify the loss of cortical responses in the left median nerve. By promptly alerting the surgeon, they facilitated quick intervention and appropriate action.
The surgeon, upon receiving the alert, was able to assess the situation and make the necessary adjustments. This may have involved repositioning or modifying the clips to restore normal sensory function. Their timely response and decision-making are vital in such cases to mitigate any potential complications.
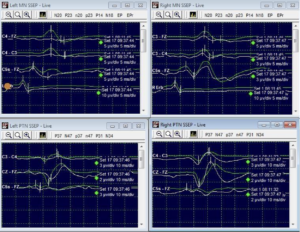
In response to the loss of cortical responses in the left median nerve, the surgeon took action by repositioning the clips that were placed on the aneurysm. This adjustment led to a significant improvement in the sensory evoked potentials (SSEP) of the left median nerve, which returned to about 50% of their initial baseline level. Additionally, the surgeon was able to successfully and satisfactorily clip the posterior communicating artery (Comm) aneurysm. This indicates that the aneurysm was properly secured, reducing the risk of further complications.
Furthermore, it is important to note that the patient did not experience any deficits or abnormalities in their neurological function after the operation. This is a positive outcome, as it suggests that the surgical intervention was effective in addressing the aneurysm without causing any adverse effects. The surgeon’s ability to reposition the aneurysm clips and restore SEP responses, combined with the absence of post-operative deficits, reflects their skill and expertise in managing such complex procedures. The patient’s favorable outcome is a testament to the surgeon’s proficiency and dedication to ensuring the best possible results.